[ad_1]
Adam Eley and Alison Holt, social affairs editor
BBC News
 BBC
BBC
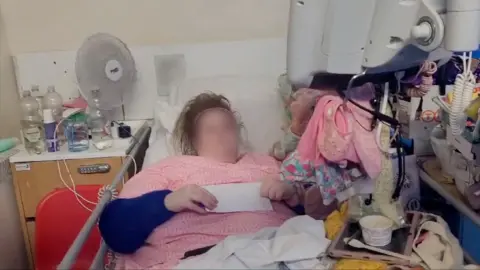
Jessie, her face blurred for privateness, within the hospital mattress the place she lived for 18 months
“I feel very angry, upset, worthless, and like my mental health and my life does not matter,” says Jessie, propped up in a hospital mattress.
She is recording this in a video diary. Blue NHS curtains are drawn across the mattress and all her possessions are stacked up within the tiny chaotic area this creates.
Among the piles of packing containers and baggage sit the dolls she holds to maintain her calm.
Thirty-five-year-old Jessie spent 550 days in Northampton General Hospital. For almost all that point, she was medically match to go away however discovering her an appropriate place to go to was tough.
The BBC has adopted her story for greater than 5 months because the NHS belief took pricey High Court motion in opposition to her, to have her evicted from the hospital mattress she was occupying.
Jessie was ultimately arrested and brought to a care house the place she says she feels anxious.
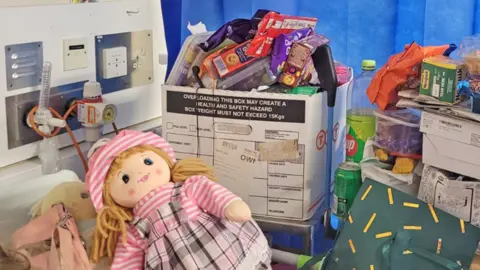
Jessie has dolls that she holds for consolation
Her story is an excessive instance, but it surely demonstrates the acute pressures confronted by a care system dealing with extra complicated instances, the knock-on impact to the NHS, and the way the individual on the coronary heart of it might probably really feel misplaced.
North Northamptonshire Council, which is liable for her housing and care, says it can’t remark due to an ongoing police investigation into Jessie’s behaviour.
The hospital says it “is not the best environment for patients who are not in need of acute medical care”.
The Department of Health and Social Care has advised the BBC: “This is a troubling case which shows how our broken NHS discharge system is failing vulnerable people.”
Jessie was one among greater than 70 individuals who contacted the BBC after studying about Matthew in Surrey – who would find yourself spending greater than a yr caught on a hospital ward earlier than being moved to a care house.
Most who wrote to us advised of their struggles to seek out the social care they wanted, some additionally confronted lengthy waits to get out of hospital.
At the beginning of January 2025, almost 13,000 out of the greater than 100,000 hospital beds in England have been occupied by individuals who did not have a medical cause to be there, in keeping with official figures.
For folks delayed for greater than every week, the commonest causes have been a scarcity of social care out there in their very own properties, or a scarcity of locations in care or rehabilitation properties.
Such delays have grow to be regular, say consultants.
Jessie’s story
It may be very uncommon for a affected person to be taken to court docket by the NHS – Jessie’s is just the fourth case since 2006. So how did she come to be arrested in her hospital mattress?
She arrived at Northampton General on 14 April 2023 needing therapy for cellulitis, a bacterial an infection affecting the pores and skin, which might be severe.
She makes use of a wheelchair and desires assist with all her private care. She has additionally been identified with an emotionally unstable persona dysfunction.
Jessie likes video games, arts and crafts, and journeys to backyard centres. She additionally finds life tough and might be difficult to these making an attempt to assist her. When careworn, she self-harms and might threaten to hurt others.
By the tip of April, she was able to be discharged from hospital, however was advised she couldn’t return to the nursing house the place she had lived for 9 years as a result of it may not meet her wants.
Jessie – who’s unable to work and reliant on advantages – grew to become more and more remoted caught inside her hospital cubicle on the six-bedded ward. She says her psychological well being deteriorated additional, folks would stare at her and he or she felt safer with the curtains drawn.

All Jessie’s possessions have been stacked up contained in the cubicle
From paperwork we’ve got seen, and from what Jessie and her mom, Hilda, have advised us, it was a couple of yr earlier than she was provided an alternate place by the native council.
Sarah Scobie, deputy director of analysis on the Nuffield Trust assume tank, says sufferers caught in hospital for 3 weeks or extra, like Jessie, have a tendency to wish numerous help, and the variety of these instances is rising.
With councils – who pay for many social care – financially squeezed and overstretched, many care properties and home-care suppliers are solely given short-term funding, she says.
It is “difficult for them to establish services, recruit staff, train staff, invest in a service, if they don’t know whether that funding is going to continue,” she provides.
The authorities says it’s offering an extra ÂŁ26bn to assist “shift the focus of care from hospital to community, and tackle delayed discharges by improving the links between the NHS and social care”.
It additionally says a assessment of grownup social care led by Baroness Louise Casey, which begins work in April, will draw up a plan for a good and inexpensive care system for the long run.
In Jessie’s case, authorized paperwork say the council investigated almost 120 care locations. Only one was provided to her.
This was a supported residing flat in a close-by city, with two care workers initially current 24 hours a day.
But the city has upsetting recollections for Jessie. She finds it too tough to speak about, aside from to say “bad things” occurred.
She advised us she was determined to go away hospital, however the considered going there made her really feel suicidal. So, she refused the one place provided.

Jessie makes use of a wheelchair and desires assist with all her private care
Under the 2014 Care Act, Jessie ought to be capable to categorical a choice about the place she lives.
She has psychological capability, however was assessed by the NHS as needing an expert advocate to help her on this, serving to her perceive the selections she is requested to make and to elucidate her views to others.
Jessie was referred to an advocacy agency by the council, however in June 2024 her case was closed after she requested for a brand new advocate however then did not reply to additional contact.
The well being and care system is “convoluted, complicated, very bureaucratic” and it’s straightforward for a affected person’s voice to get misplaced, says Caroline Entwistle from the advocacy charity, VoiceAbility.
She believes an advocate can “take that pressure off the person who’s feeling quite overwhelmed” – however that funding for such companies shouldn’t be maintaining with demand.
The hospital did present Jessie with psychological well being help whereas she was in her cubicle. But she believed no-one was listening to her.
“I explained all the reasons I wasn’t happy with [the accommodation],” she says, “but they just went ahead with it anyway.”
In August 2024, 16 months after she arrived, the hospital began authorized motion in opposition to Jessie to repossess the mattress she was in.
She didn’t actually perceive what was occurring, she says. Neither did her mom. They couldn’t discover a solicitor and had no advocate, so the primary two hearings went forward with out anybody representing Jessie’s views.
The NHS belief argued a affected person did not have the suitable to decide on their placement, and {that a} hospital mattress took up important useful resource.
It mentioned it had taken account of Jessie’s vulnerabilities all through and the package deal of care provided by the council was important, with workers current 24 hours a day to maintain her secure.
A care plan, which detailed the help Jessie wanted, was solely given to the court docket on the closing listening to. The date suggests the evaluation was accomplished the day earlier than. It additionally notes that “Jessie is unable to communicate effectively”.
At the ultimate High Court listening to on 4 October, Jessie attended remotely from hospital. Within minutes she was overwhelmed and needed to depart. Her mom struggled to talk for her.
The choose mentioned Jessie may problem the council’s evaluation of whether or not the lodging and care have been proper for her, however she couldn’t stay in hospital “when she does not need a bed there, and has not needed one for over a year, and others do”.
He dominated that Jessie should depart hospital, and mentioned “we must hope the transition goes smoothly”.
The hospital belief says it’s dedicated to working with “care partners to provide the best possible care for those in our communities” within the place that “best suits their needs”.
The most up-to-date information, from 2020-21, suggests an ordinary NHS hospital mattress prices ÂŁ345 per day. Adjusting for inflation, this could imply Jessie’s hospital keep is more likely to have value greater than ÂŁ200,000. We have no idea how a lot the authorized motion value.
Ten days after Jessie’s closing listening to, 18 months after she arrived in hospital, the police arrested her. She spent a number of hours at a police station earlier than being moved to the flat within the city that holds unhealthy recollections.
Police are investigating her for numerous alleged incidents, she advised us, together with for sending offensive emails shortly earlier than she was evicted in October.
Since transferring, Jessie says she has self-harmed and the police have been referred to as on three events – as soon as by Jessie, twice by workers.
“They don’t know what to do with me,” she says.
Jessie has just lately been visited by a brand new advocate.
[ad_2]



